FOTODUETS/ISTOCK/GETTY IMAGES PLUS
FOTODUETS/ISTOCK/GETTY IMAGES PLUS
Benign Paroxysmal Positional Vertigo After Osteotome Use In Maxillary Dental Implant Placement
This rare complication involving osteotome use in dental implant procedures can be managed with the Epley maneuver.
Benign paroxysmal positional vertigo is a condition where dislodged otoliths from the utricle or saccule of the ear enter into the semi-circular canal, resulting in the inappropriate movement of the endolymph. In turn, this movement of the endolymph leads to symptoms of vertigo, nausea and postural imbalance.1
Benign paroxysmal positional vertigo can be caused by a variety of sources, such as head injuries, vascular disorders, trauma and infection.2 In certain cases, oral surgery procedures can result in this complication, such as when osteotomes are used to prepare implant osteotomies.3 The percussion of osteotomes can detach the otoliths from the otoconia layer and displace them into the posterior portion of the semicircular canal.3
Although complications from osteotome procedures are relatively rare,4 the symptoms of benign paroxysmal positional vertigo can be quite debilitating. Despite the self-limiting nature of the condition,5 the symptoms often lead patients to seek treatment. One of the most effective and noninvasive ways to treat benign paroxysmal positional vertigo is by a canalith repositioning procedure, also known as the Epley maneuver.6
This report describes the symptoms and management of a 64-year-old Caucasian male without a previous history of vertigo who experienced benign paroxysmal positional vertigo after a dental implant procedure that involved the use of osteotomes.

CASE DESCRIPTION
The patient presented for placement of four dental implants. He had lost his maxillary teeth earlier that same year, had a full denture, and was looking for improved denture support.
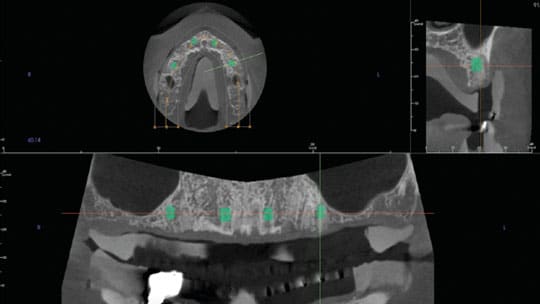
A medium-field-view cone beam computed tomography (CBCT) scan was acquired with a 3D scanner (90.0 kV, 8.0 mA and 17.5 s) and reconstructed at a size of 0.16-mm voxel. The CBCT scan was interpreted by a board-certified oral and maxillofacial radiologist. The edentulous maxillary arch exhibited severe residual ridge resorption of the molar areas bilaterally. Moderate residual ridge resorption was observed in the bilateral premolar area and anterior maxilla. No bony sinus septation or maxillary ridge irregularity was observed in the areas of missing teeth. Simulated dental implant planning and placement was conducted utilizing planning software (Figure 1 and Figure 2). Based on the treatment plan, it was decided to place four endosseous dental implants in sites #4, 6, 11 and 13, all of which presented with Type III bone (Lekholm and Zarb classification).7 Due to the minimal bone density estimated (based on CBCT imaging), it was decided to utilize osteotomes for lateral condensation of the maxillary bone when preparing the implant sites.
On the day of the procedure, a mid-crestal incision was made around the maxillary arch from first molar to first molar. Full thickness flaps were developed both palatally and buccally. In site #4 the patient had a bone ridge height of 7.4 mm and a width at the bone crest of 7.5 mm. In this site, a 5-mm-diameter, 6-mm-long implant (coating: CaPh/Ha) was placed. In site #6, the patient had a bone ridge height of 10.9 mm and a width at the bone crest of 5.7 mm. In this site, a 3.5-mm-diameter, 8-mm-long implant (coating: CaPh/Ha) was placed. In site #11, the patient had a bone ridge height of 16.6 mm and width at the bone crest of 6.0 mm. In this site, a 3.5-mm-diameter, 8-mm-long implant (coating: CaPh/Ha) was placed. In site #13, the patient had a bone ridge height of 9.5 mm and width at the bone crest of 7.7 mm; here, a 4.5-mm-diameter, 6-mm-long implant (coating: CaPh/Ha) was placed.
Each implant osteotomy was prepared with a series of progressively wider osteotomes to condense the bone laterally. Implants were then tapped into place according to the implant manufacturer’s protocol.8 After the implants were placed, the incisions were closed primarily with 3.0 absorbable suture material using a vertical mattress and continuous interlocking suture technique. The procedure lasted two hours. Final results from the procedure can be seen on the panoramic radiograph in Figure 3.
The night of the procedure, the patient reported experiencing vertigo when ambulating. The patient also complained of “spinning” when lying in bed, which led to nausea and insomnia. The next evening, the symptoms of vertigo and nausea worsened. The patient also reported a tendency to lean to the right and fall over due to the loss of balance. The next morning, the patient returned to the clinic and reported symptoms of vertigo. The treating surgeon made a diagnosis of benign paroxysmal positional vertigo secondary to the use of osteotomes. Recommendation was given to see an otolaryngologist to verify the diagnosis and recommend treatment. The patient talked to his son, a physician, who recommended the Epley maneuver before seeing an otolaryngologist. The patient performed the Epley maneuver and had immediate relief. At the one-week follow-up, he reported the absence of vertigo and nausea.

The Epley maneuver was first described by John M. Epley, MD, in 1980.9 In the procedure, a patient’s head is turned 45 degrees while sitting in an upright position; next, the physician passively shifts the patient supine, from which the individual hold his or her head 30 degrees in extension in three different positions for 30 seconds, shifting the head more and more toward the affected side10 (Figure 4). This maneuver is effective at alleviating benign paroxysmal positional vertigo 70% of the time upon first treatment, and nearly 100% of the time with successive treatments.10 Holding the head in the various positions allows the otoliths to reposition back to the saccule and utricle of the inner ear, alleviating nausea and vertigo.10,11
DISCUSSION
In this case, osteotomes were utilized for implant site development. This was performed in an effort to facilitate implant placement and primary implant stability due to the patient’s Type III bone (Lekholm and Zarb classification).7 It has been shown that this technique can result in increased primary stability of implants in bone which is less dense.12 It has also been shown that benign paroxysmal positional vertigo can result from the use of osteotomes in preparing implant sites, as was done in this case.3 The implant manufacturer’s protocol8 for placement also calls for the use of a mallet to place the implants into the alveolar bone. This, too, creates percussive forces and therefore must be considered a possible contributing factor to the patient’s benign paroxysmal positional vertigo.
In mildly resorbed maxillary bone, a sinus floor elevation is often performed to provide adequate bone height at the time of implant placement.13 Among the various techniques to accomplish this are the osteotome sinus floor elevation (OSFE)14 and reamer sinus floor elevation.15 In comparing the efficacy of these two techniques, there is no significant difference.15 However, when comparing possible postoperative complications, such as dizziness, headache, bleeding and benign paroxysmal positional vertigo,4,15 OSFE has more than twice the incidence (15.6%).15
A possible explanation for the vestibular complications seen with OSFE is the use of percussive force.16 With OSFE, the use of a surgical mallet and osteotomes can transmit enough force to detach heavy otoliths from the otoconia layer.3,16

CONCLUSION
This case is of interest due to the fact this complication is relatively rare in dental implant procedures.16 Therefore, practitioners using the osteotome technique to place implants may not be aware of the risk, or how to mitigate it. They should also be aware of alternative techniques that can deliver the same outcome. The risk of developing benign paroxysmal positional vertigo with procedures involving the use of osteotomes can be diminished with several tactics. First, by reducing the amount of percussive force utilized with the mallet and osteotomes. Second, hyperextension of the patient’s neck should be minimized. Lastly, a thorough history to rule out previous episodes of vertigo is important, as such patients are believed to be more susceptible to benign paroxysmal positional vertigo.17 Practitioners should also consider utilizing alternative techniques to condense Type III bone in preparation for dental implant placement. One alternative is through the use of osseodensification burs, which have been shown to increase primary stability and bone mineral density.18 However, if vertigo is still experienced after the placement of maxillary dental implants, the Epley maneuver is a viable treatment option,10 along with referral to an otolaryngologist.
KEY TAKEAWAYS
- Although it is a rare complication, oral surgery procedures can produce benign paroxysmal positional vertigo — such as when osteotomes are used to prepare implant osteotomies.3
- Symptoms of benign paroxysmal positional vertigo can be quite debilitating.
- One of the most effective and noninvasive ways to treat benign paroxysmal positional vertigo is with a canalith repositioning procedure, also known as the Epley maneuver.6
- Holding the head in the various positions allows the otoliths to reposition back to the saccule and utricle of the inner ear, alleviating nausea and vertigo.10,11
- The Epley maneuver is effective at alleviating benign paroxysmal positional vertigo 70% of the time upon first treatment, and nearly 100% of the time with successive treatments.10
- See the text for additional approaches that can help mitigate the risk for benign paroxysmal positional vertigo resulting from dental implant procedures.
REFERENCES
- Hall SF, Ruby RR, McClure JA. The mechanics of benign paroxysmal vertigo. J Otolaryngol. 1979;8:151–158.
- Baloh RW, Jacobson K, Hondrubia V. Horizontal semicircular canal variant of benign positional vertigo. Neurology. 1993;43:2542–2549.
- Penarrocha M, Perez H, Garcia A, Guarinos J. Benign paroxysmal positional vertigo as a complication of osteotome expansion of the maxillary alveolar ridge. J Oral Maxillofac Surg. 2001;59:106–107.
- Di Girolamo M, Napolitano B, Arullani CA, Bruno E, Di Girolamo S. Paroxysmal positional vertigo as a complication of osteotome sinus floor elevation. Eur Arch Otorhinolaryngol. 2005;262:631–633.
- Su GN, Tai PW, Su PT, Chien HH. Protracted benign paroxysmal positional vertigo following osteotome sinus floor elevation: a case report. Int J Oral Maxillofac Implants. 2008;23:955–959.
- Li JC, Li CJ, Epley J, Weinberg L. Cost-effective management of benign positional vertigo using canalith repositioning. Otolaryngol Head Neck Surg. 2000;122:334–339.
- Lekholm U, Zarb GA. Patient Selection and Preparation In: Brånemark PI, Zarb GA, Albrektsson T, eds. Tissue-Integrated Prostheses: Osseointegration in Clinical Dentistry. Chicago: Quintessence Publishing Co; 1985:199–209.
- Bicon Dental Implants. Two Stage Surgical Technique: Keys to Success. Available at: http://www.bicon.com/tech/t_SM_sp02.html. Accessed September 5, 2019.
- Epley JM. New dimensions of benign paroxysmal positional vertigo. Otolaryngol Head Neck Surg. 1980;88:599–605.
- Muncie HL, Sirmans SM, James E. Dizziness: approach to evaluation and management. Am Fam Physician. 2017;95:158–159.
- Herdman SJ. Treatment of benign paroxysmal positional vertigo. Phys Ther. 1990;70:381–388.
- Shayesteh YS, Khojasteh A, Siadat H, et al. A comparative study of crestal bone loss and implant stability between osteotome and conventional implant insertion techniques: a randomized controlled clinical trial study. Clin Implant Dent Relat Res. 2013;15:350–357.
- Kim MS, Lee JK, Chang BS, Um HS. Benign paroxysmal positional vertigo as a complication of sinus floor elevation. J Periodontal Implant Sci. 2010;40:86–89.
- Summers RB. A new concept in maxillary implant surgery: the osteotome technique. Compendium. 1994;15:152,154–156,158.
- Bae OY, Kim YS, Shin SY, Kim WK, Lee YK, Kim SH. Clinical outcomes of reamer- vs. osteotome-mediated sinus floor elevation simultaneous implant placement: a 2-year retrospective study. Int J Oral Maxillofac Implants. 2015;30:925–930.
- Saker M, Ogle O. Benign paroxysmal positional vertigo subsequent to sinus lift via closed technique. J Oral Maxillofac Surg. 2005;63:1385–1387.
- Su GN, Tai PW, Su PT, Chien HH. Protracted benign paroxysmal positional vertigo following osteotome sinus floor elevation: a case report. Int J Oral Maxillofac Implants. 2008;23:955–959.
- Huwais S, Meyer EG. A novel osseous densification approach in implant osteotomy preparation to increase biomechanical primary stability, bone mineral density, and bone-to-implant contact. Int J Oral Maxillofac Implants. 2017;32:27–36.
The authors have no commercial conflicts of interest to disclose.
From Decisions in Dentistry. October 2019;5(9):9–10,12.